Arkansas Telehealth Partnership Reduces Stroke-Related Deaths
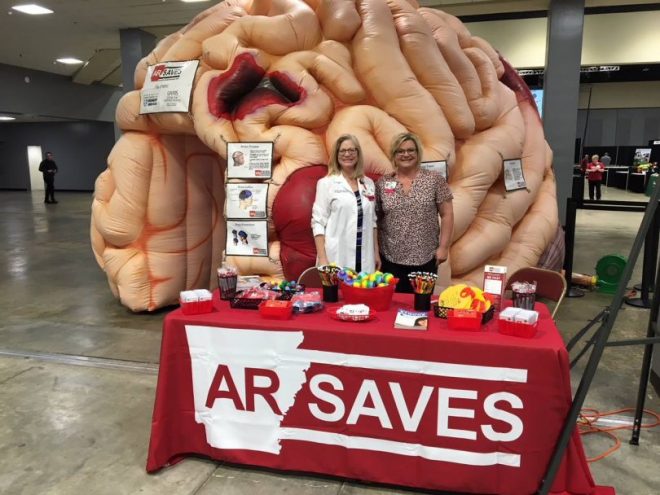
The AR SAVES partnership established a broad hospital-based telehealth network and is testing first responder technologies to improve stroke response.
Hospitals that have stroke center prides themselves on their door-to-needle times — the minutes from when a stroke patients first enters the ER to when they are properly diagnosed and begin receiving “clot-busting” tissue plasminogen activator (tPA) treatment.
A 25-minute door-to-needle time saved my life when I had a stroke in 2015. But what if the person having a stroke lives hours away from the nearest hospital that can provide treatment?
The University of Arkansas Medical Services (UAMS) is using public broadband and an established telehealth network to tackle this major challenge with a new telestroke pilot underway that could further enhance the state’s stroke response.
How an Arkansas Government Partnership is Reducing Stroke-Related Deaths
Arkansas used to lead the United States in stroke deaths. Less then 1 percent of stroke patients statewide received the de-clotting drug alteplase (tPA). It’s one of 11 states that make up the “stroke belt,” where there is a higher prevalence of stroke and stroke-related death.
In 2008, the Arkansas Department of Human Services partnered with the Center for Distance Healthat UAMS to form Arkansas Stroke Assistance through Virtual Emergency Support (AR SAVES). This telecom-stroke program was instrumental in the state’s ability to reduce stroke-related deaths with Arkansas dropping to number 7 on the 2016 list of stroke deaths by state.
Currently, 54 of the 80 hospital statewide participate in AR SAVES.
“We’ve gone from 1 percent to 33 percent of stroke patients in those 54 hospitals are now qualified for the program to receive tPA,” said Roy Kitchen, Arkansas e-Link Director.
The remaining patients either did not suffer severe enough strokes for the medication, or decided to seek treatment elsewhere.
Arkansas Creates Statewide Healthcare Hub Publicly-Owned Fiber Backbone
The telehealth strategy that underlies UAMS’ telestroke program is applicable to both urban and rural communities.
Tina Benton, Director of the Center for Distance Health noted it may be one of the only hospitals in the United States to provide “a statewide telemedicine application that crosses over multiple hospital systems.”
AR SAVES operates across a public-owned fiber backbone called Arkansas Research Education Optical Network (ARE-ON). ARE-ON owns a statewide high-speed fiber optic backbone network with 1 Gigabit and 10 Gigabit ethernet connections.
Each hospital has its own clinical equipment for the telemedicine operations. A number of healthcare providers also can connect with nearby small clinics for video consults or other services.
Arkansas’s Telehealth Strategy a Model for Cities and Counties
Although AR SAVES is a statewide program, local communities can emulate the state university’s operations.
ARE-ON is a statewide network. Some states may have similar networks, such as the Corporation for Educational Network Initiatives in California (CENIC). CENIC has partnered with the California Telehealth Network (CTN) that provides connectivity and telehealth services to hundreds of healthcare facilities throughout the state.
But locally, hundreds of municipalities and co-op have built, or are building, community-owned broadband networks that can be great platforms for telehealth. Their numbers are increasing.
Whenever they can, communities are opting to own their own broadband, partner with other cities or co-ops that already have networks or form public private partnerships. The FCC and the U.S. Department of Agriculture provide funds to local hospitals to build broadband infrastructure.
Once a community has a telestroke operation in place, what comes next? Kitchen advises them to look for appropriate partnerships.
Benton cited explosion accident response as an example. “We will partner with other health and telehealth programs, including a huge trauma care program. If there was a big explosion near one of the hospitals, that’s where patients could be triaged and treated in consultation with specialists at other hospitals via telemedicine. There are only 16 burn injury beds in Arkansas, so they use telemedicine to triage treatment for these injuries,” she said.
A city or county should do a needs assessment to determine the best telehealth strategy.
For example, a hospital in Iowa recently announced they were going to stop delivering babies. The communities in that region may look to telehealth to provide prenatal care. UAMS’ telehealth services actually started before AR SAVES with providing care for women with high-risk pregnancies.
Assessment includes cost analyses.
“If someone injured their hand on a farm or in an industrial plant, they would be sent by helicopter to our hospital, we’d check them and send them home to wait for a doctor to schedule them for a visit,” said Benton.
The helicopter costs $30,000 per trip, she addded, so UAMS partnered with the Arkansas Trauma Communications Center (ATCC) to create an orthopedics hand injury program.
Communities also can view telehealth as a vehicle to impact local economies as well as provide healthcare services.
Benton and Kitchen work with others to determine what types of services enable patient to stay close to home throughout their care and recovery. AR SAVES provides a 24 hour on-call service with a stroke center neurologist. A patient can stay at the local hospital where they initially are admitted.
First Responder Vehicle Tech Enhancements Could Reduce Arkansas’ Stroke-Related Deaths
AR SAVES recently launched a pilot test to outfit ambulances and other first responder vehicles with wifi hot spots and other technology to ambulances in an effort to improve stroke response in remote areas.
“Some of our rural homes may be two or three hours from the nearest hospital,” said Joiner.
Giving an EMT a direct video connection to the stroke center enables doctors to start life-saving treatment while enroute to the hospital.
“A stroke patient has a three-hour window for receiving treatment, or the consequences of a stroke can be much worse or fatal,” she said.
Benton and Kitchen Kitchen are exploring UAMS innovations in telehealth and telemedicine with the National Telecommunications and Information Administration.
Article original posted via Efficientgov.com
